Nursing, along with the rest of the medical field, is constantly evolving to ensure better patient outcomes. Nursing skills, in particular, have changed quite a bit over the last several decades. Some skills have even been discarded completely for the sake of safety or efficiency. Here are 10 interesting examples of old-school nursing skills that have either drastically changed or are no longer practiced:
- Reusing syringes and urinary catheters
Believe it or not, new nurses, many of today’s disposable medical items, like urinary catheters and syringes, were made to be reused in the not-too-distant past. These items were sterilized between uses, a process that was eventually deemed too costly as disposable items became more common.
- Charting patient care on paper
While it’s still possible to find rural and small-scale clinics that utilize paper charting, the majority of health-care facilities these days chart electronically. In addition to providing all members of the health-care team with easier access to patients’ charts, electronic charting is typically more efficient and more accurate.
- Using urine dipsticks with sliding-scale insulin
Sliding-scale insulin has been in use longer than glucose meters. Before these meters were used to determine how much, if any, insulin to administer to a diabetic patient, nurses had to rely on urine dipsticks. Urine-dipstick results aren’t as accurate as those provided by glucose meters, so it’s no surprise that they aren’t used in this manner anymore.
- Regulating IV fluids manually
Before infusion pumps were invented, it was necessary to manually regulate IV fluids. To do this, nurses had to count drops and calculate drip rates for each and every patient receiving IV fluids. Now, thanks to infusion pumps, administering IV fluids is easier, more accurate, and much faster.
- Palpating for blood pressure
The vast majority of health-care facilities throughout the United States take patients’ blood-pressure measurements automatically, but this wasn’t always the case. Nurses used to rely on palpation to obtain blood-pressure measurements. To obtain a patient’s blood pressure in this manner, nurses would inflate and deflate a compression cuff while feeling for the disappearance and reemergence of the radial pulse.
- Shaving patients prior to surgery
Up until fairly recently, hairy patients had their incision sites shaved prior to surgery. New evidence suggests that this leads to an increased risk of infection, and many hospitals have eliminated this practice. Now, instead of using a razor, nurses use clippers to cut away excessive hair as a part of their preoperative preparations.
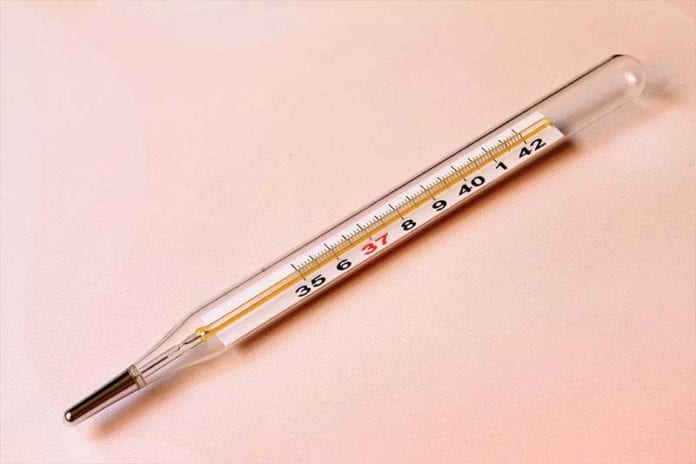
- Shaking mercury thermometers
Now that digital thermometers are used to obtain patients’ temperatures, the sight of a nurse shaking a mercury thermometer is extremely rare. In the past, however, nurses could be seen shaking mercury thermometers in hospitals on a daily basis. The reason that these old-school thermometers were shaken is that the mercury would often cling to the inner sides of the thermometer. Prior to taking a new temperature reading, bringing the majority of the mercury back down into the bulb by shaking the thermometer was the best way to ensure accuracy.
- Cutting urinary catheters during removal
While cutting urinary catheters during removal is not recommended, some nurses and doctors still utilize this practice. It’s considered unsafe for two reasons primarily. Firstly, traction on the catheter could cause it to retract into the bladder if it’s cut. Secondly, the balloon might not deflate, which turns a simple catheter removal into something much more difficult and costly.
- Irrigating NG tubes with Coca-Cola
Many old-school nurses swear by Coca-Cola for NG tube flushing. In theory, this is due to the coke’s acidity. Regardless of the reason behind this method’s supposed effectiveness, it’s not recommended as it can affect the plastic tubing. Before using coke, juice, or something similar to flush an NG tube, refer to your facility’s guidelines. More likely than not, using water when flushing an NG tube will be the preferred method.
- Treating congestive heart failure (CHF) with rotating tourniquets
CHF patients used to be treated with rotating tourniquets. Essentially, these tourniquets were applied to the lower limbs to diminish venous return. These days, however, we have a wide variety of effective diuretics that can be used to help decrease the strain that excess fluid volume puts on the heart. Not only is this treatment more comfortable for patients than applying tourniquets, it’s much more effective.
Are there any old-school nurses working with you on your unit? If so, do they still practice a few of the skills mentioned in this article? Leave a comment below and let us know!


BEING A NEW GRAD IN 1970, I PERFORMED ALL OF THOSE MENTIONED SKILLS AND OVER MY 43+ YRS IN THE PROFESSION SAW NUMEROUS CHANGES. SOME VERY GOOD AND SOME NOT AS EFFECTIVE BUT USEFUL. I ALSO BELIEVE SOME OF THE “OLD SCHOOL” SKILLS NEED TO BE KEPT IN MIND WHEN TEACHING STUDENTS IN TIMES OF EMERGENCY OR FOR SYSTEMS FAILURES.
One big change you failed to mention is the pre-HIV era when there was no such thing as universal precautions and I remember patients pulling out IV’s and I would apply pressure with ungloved hands and never thought anything of it.
I did every one of these when I first became a nurse in 1975. It is wonderful to see how far we have come and I look forward to where medicine is going.
Ahww..the good old days! Truthfully, now when the computers go down, its a pain to paper chart, even tho I did it for years!! To tranfer a sick newborn, we had to place a sheet of carbon paper between our papers to be able to send a “copy” to the accepting hospital!! Good times, good times…
When I first became a nurse – 42 years ago – everyone had a turn as the Diabetic Nurse; which we all hated. Before dipsticks for diabetic testing there were “diabetic urine test kits”. They contained 2 small test tubes and testing tablets. You had to collect urine from all the diabetic patients; go to the dirty utility room; line/set up the urine with the correct patient kit. Put urine in test tubes; drop tablet in urine; watch for color change & compare to color chart to figure out how much insulin to give. When there were 10 or more patients on your unit it took forever.
So thankful for glucometers!!!!!!!!
A couple of these are still important skills to have in case of e. g. power failure, system failure or going on a medical mission to a “low-tech” country. Legible handwriting not least of these. As an old-school ED nurse I strongly insist on the importance of being able to palpate a BP.
I am guilty of shaking the electronic thermometer on the vital signs machine during nursing school …… right after I placed the plastic sheath on it ….. my professor was there because it was my first vital sing done in clinicals. The plastic flew across the room. The patient was a seasoned nurse and thought this was the funniest thing she ever saw a new nursing student do. My professor just stared at me and said “critical thinking skills Bonnie!” . I was so embarrassed.
Some outdated protocols are welcomed like reuse of syringes. I like the fact that now we can read what the doctor actually orders because we have computerized charts. What a blessing.
Now on the flip side as a patient people are missing out on the PM back rub especially after having a baby and you were pampered in the hospital for 3 days before discharge.
I used to enjoy back rub time as much as the patients. You can learn a lot about what is going on in their world during that little time.
Bed baths and back rubs was standard pm care. A new nurse would just laugh if a patient asked for a back rub
OMG, I could definitely relate to each of those!
Especially rotating tourniquets, What a night mare~!